What is a Tooth Abscess?
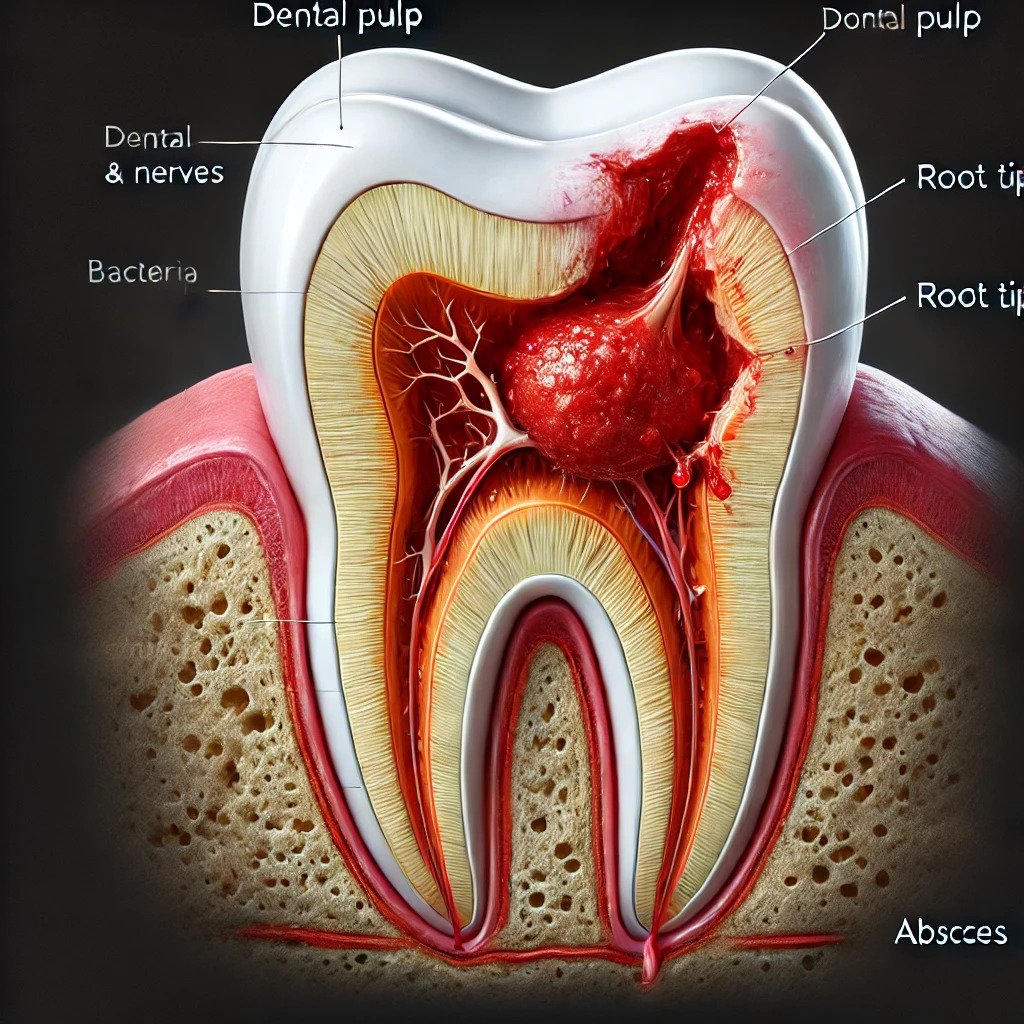
A tooth abscess is a painful pocket of pus caused by a bacterial infection. It can form in various areas near the tooth, often resulting from untreated dental cavities, decayed or fractured teeth, injuries, or prior dental work. The infection leads to irritation, swelling, and inflammation that may involve the gums, roots, and surrounding bone. Bacteria can enter the innermost pulp through a deep cavity, chip, or crack, spreading to the blood vessels and tissues. If left untreated, this condition can lead to significant complications. A tooth abscess often presents as a red, swollen bump resembling a boil or pimple and can cause severe pain that may spread to neighboring teeth.
Types of Tooth Abscesses
Periapical Abscess (per-e-AP-ih-kul):
Occurs at the tip of the root when bacteria spread to the pulp through a deep cavity, fractured tooth, or decay.
Affects the innermost nerves and blood vessels, leading to pus formation in the surrounding bone.
Can cause intense pain and serious damage if left untreated.
Periodontal Abscess (per-e-o-DON-tul):
Found in the gums and surrounding tissues.
Commonly associated with gum disease.
Occurs when pus forms around the roots, causing swelling and inflammation in the supporting structures of the tooth.
Gingival Abscess:
Develops on the gums without usually affecting the supporting structures of the tooth.
Often caused by foreign objects getting stuck in the gums, leading to localized irritation and infection.
Signs and Symptoms
Common signs of a tooth abscess include:
- Severe, constant, or throbbing toothache that may radiate to the jawbone, neck, or ear.
- Increased pain with exposure to hot or cold temperatures or during chewing.
- Swelling in the face, cheek, or neck; tender swollen lymph nodes in the jaw or neck.
- Fever and a general feeling of discomfort or uneasiness.
- Foul odor in the mouth or bad breath (halitosis).
- A sudden rush of foul-smelling fluid in the mouth if the abscess ruptures, often providing temporary relief.
- Visible redness and swelling in the gums, sometimes with a draining sore near the affected tooth.
- Increased sensitivity to temperature changes and pressure; sometimes accompanied by a bitter taste.
- Loosening of the affected tooth or difficulty opening the mouth.
- Pus drainage from the abscess.
Causes
A tooth abscess typically develops due to a periapical infection, where bacteria invade the innermost part of the tooth—the dental pulp. This core contains blood vessels, nerves, and connective tissue. Bacteria can enter through:
- Severe cavities that destroy the tooth’s hard surface due to acid production from bacteria breaking down sugars.
- Broken, chipped, or cracked teeth that allow bacteria to seep into deeper layers.
- Periodontal disease that enables bacteria to invade deeper structures as it progresses.
- Injury or trauma to the tooth that may not show visible damage but makes it susceptible to infection.
Risk Factors
Certain factors increase your risk of developing a tooth abscess:
- Poor oral hygiene practices such as infrequent brushing and flossing can lead to serious dental issues like cavities and gum disease.
- A diet high in sugar contributes to dental cavities that can evolve into an abscess.
- Dry mouth conditions reduce saliva production (often due to medications or aging), increasing susceptibility to decay.
Tips for Prevention
To avoid developing a tooth abscess:
- Maintain good oral hygiene: Brush your teeth for two minutes at least twice daily using fluoride toothpaste. Don’t forget to floss daily.
- Replace your toothbrush every 3 to 4 months or sooner if bristles are frayed.
- Consider using an antiseptic or fluoride mouth rinse for additional protection.
- Drink water containing fluoride to strengthen enamel and prevent decay.
- Eat a balanced diet low in sugar and limit between-meal snacks.
- Schedule regular dental checkups for professional cleanings and early intervention if any issues arise.
FAQs
Can a tooth abscess go away on its own?
A tooth abscess won’t heal on its own and requires treatment. If the abscess ruptures, you might feel significant pain relief, leading you to believe the issue is resolved — but dental care is still necessary. Without proper treatment, an undrained abscess can allow the infection to spread to your jaw, head, or neck, causing serious complications.
How serious is a tooth abscess?
If a tooth abscess is not treated, the infection can spread to your jawbone, the soft tissues in your face and neck, and even further. In very rare cases, it may reach your heart (endocarditis) or brain (bacterial meningitis), leading to severe complications.
Will antibiotics get rid of a tooth abscess?
In cases of severe infection, the affected tooth may need to be extracted. However, early treatment can often eliminate the infection and preserve the tooth. Antibiotics alone cannot cure a tooth abscess; it requires proper care from a dentist or dental professional.


